Serotonin (5-hydroxytryptamine, 5-HT) is a neurotransmitter that is involved in just about everything. It helps ensure proper cell growth, maturation and migration during development. Serotonin is also important in regulating emotions, cognitive functions, appetite, pain, circadian rhythms, and our endocrine system in adulthood. It is hardly a surprise then, that the serotonergic system seems to be important in bulimia nervosa (BN).
I’ve written previously about serotonin in restricting-type anorexia nervosa, so for this post I’m going to be shifting focus and talk about bulimia and binge-purge type anorexia nervosa (AN-BP).
The information in this post isn’t coming from a review paper. Instead, I’m going to be summarizing and explaining information from a chapter in a book titled Behavioural Neurobiology of Eating Disorders. In the chapter on serotonin and bulimia, Howard Steiger and colleagues propose a model for serotonin action in bulimia nervosa which takes into account “diverse hereditary and environmental influences… and helps account for heterogeneous traits seen in the bulimic population“.
Individuals whose eating disorders are characterized by the presence of binge-eating and purging display a range of temperamental traits, but the intensity and the number of traits vary from person to person. In other words, no two BN or binge-purge AN patients are the same, and many can be really different. Of course, this makes it difficult to understand (and to study) the factors that lead individuals to engage in binge-eating and purging behaviours.
This means that you’ll likely see lots of contradictory studies or mutually exclusive theories about serotonin function in bulimia – and eating disorders in general. This is normal in any young field – and neurobiology and genetics of EDs is a very young field. It may be that some of what we (and by “we”, I mean scientists) think about EDs is wrong, but a more likely alternative (if contradictory studies are methodologically sound) is that a lot of things are right (or true), but perhaps for a specific subset of this heterogeneous population (for example, someone with comorbid borderline personality disorder might have very different BN etiology compared to someone with a long history of AN and no psychiatric comorbidities.) My point with this diversion is mainly to remind readers that science is a process and not a collection of facts and some bits of knowledge have more empirical support than others.
Okay, anyway, let’s get back to the topic of serotonin and bulimia.
According to several studies, individuals with bulimic symptoms can be – very roughly – categorized into three groups: about a third are highly emotional, impulsive, and dis-inhibited (“dysregulated”); another third is detail-oriented, compulsive and has difficulty switching cognitive thinking patterns (“over-regulated”); and the last third is “quite free of observable psychopathology”.
These differences likely play a role in the etiology (causes), clinical presentation and course of the disorder. They may also – at least in part – explain the variability in treatment outcomes (why does CBT work for some, but not for others?) My hunch is that the “over-regulated” group is probably more likely than the “dysregulated” group to have suffered from anorexia nervosa prior to BN.
Some things we know about the role of serotonin are well-established, whereas others are more controversial (which often means there are contradictory studies in the literature).
Serotonin appears to be important in mediating harm assessment and harm avoidance. (In psychology, the term “harm avoidance” is much more complex than the literal definition of avoiding harm, it includes traits such as “excessive worrying; pessimism; shyness; and being fearful, doubtful, and easily fatigued”.) Decreasing serotonin neurotransmission is correlated with an inability to inhibit responses and “adopt cautious waiting attitudes.”
Less well-established is the association of increased serotonin neurotransmission with behavioural inhibition, compulsiveness, inflexibility and enhanced vigilance. The inconsistencies may be due to faulty methodology in some studies, or perhaps due to the fact that maybe serotonin is less important in mediating these traits.
Low levels of serotonin are associated with a propensity toward “impulsive aggression, suicidality, and self-injuriousness”.
The next obvious question is: what regulates the level of serotonin in the brain?
As it turns out (and I apologize for the repetition for those who have read my previous post on serotonin), food is a crucial source of serotonin. Okay, not exactly serotonin but a precursor to serotonin – the molecule that is required to make serotonin – tryptophan. Tryptophan is an essential amino acid, which means our bodies cannot produce it: we must get it from food.
Interestingly, decreased tryptophan levels in the brain (and thus the synthesis of serotonin) increases bulimic urges (or depression) in bulimic and recovered bulimic individuals. (A similar study in AN patients have found that acute tryptophan depletion is anxiolytic – or anxiety reducing. Of course, one study is hardly enough – I know more have been done, but I need to read more about acute tryptophan depletion to get a better sense of where the consensus lies.)
And here we come across a hint as to why bulimia is more prevalent in females than males (and this likely extends to eating disorders more generally).
Furthermore, given disproportionate occurrence of bulimic syndromes in females, it is noteworthy that interventions aimed at lowering 5-HT activity (e.g., a 3-week calorie-reducing diet or acute tryptophan depletion) will produce greater alterations of 5-HT function or lowering of mood in women than in men (Goodwin et al. 1987; Young and Leyton 2002). In other words, dietary effects upon 5-HT activity seem to preferentially affect females.
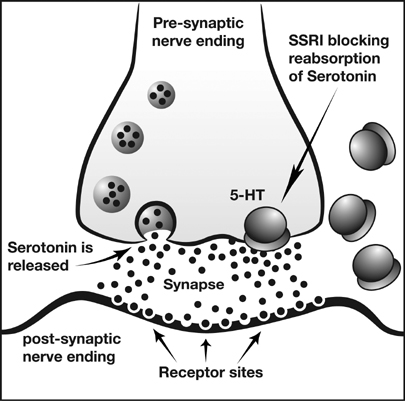
There’s been a lot of studies trying to identify different variants (called polymorphisms) of genes involved in the serotonin pathway that are associated with eating disorders or traits known to involve serotonin (harm avoidance, neuroticism, impulsivity). These polymorphisms are different versions of a gene (think different eye colour or blood types). For example, alterations in a gene that makes the serotonin transporter protein – required to get serotonin back into the cell it was released from and stopping neurotransmission – may change how fast the protein uptakes serotonin back into the cell. So, effectively, regulating how much and how long serotonin gets to bind to the other cell, even if the same amount of serotonin is released, can lead to very different downstream effects in individuals with different versions of this gene.
I’m not going to bore you with all the findings, as they are generally inconsistent. (Suggesting serotonin influences many different traits and is not specific to any trait in particular.) But one thing that is clear is that people with bulimia (and those who have recovered from bulimia) have alterations in the serotonin system. In fact, it is also often altered in unaffected relatives of BN patients (not much surprise here).
Here are some more details on the alterations in the serotonergic system in BN:
“(a) reduced central 5-HT transporter availability in women with BN (Tauscher et al. 2001) or who have recovered from bulimic anorexia nervosa (AN) (Bailer et al. 2007);
(b) reduced 5HT2a receptor binding (in subgenual cingulate, mesial temporal, and parietal cortical regions) in women recovered from BN (Bailer et al. 2004);
(c) increased presynaptic 5-HT1A autoreceptor activity (in the dorsal raphe) of people recovered from bulimic-type AN, and in postsynaptic 5HT1A receptors in various brain regions in people with active BN (Tiihonen et al. 2004).”
Research on nonhuman primates has shown that a particular version of the serotonin transporter gene (the one that gets serotonin back into the releasing (or presynaptic) cell), termed the “low-function” allele, alters stress-response (and serotonin metabolism). The “implication is that developmental stress, in genetically susceptible individuals, can precipitate alterations in [serotonin] activity”. (Alleles are alternative forms of a gene – again, think blood types and eye color.)
Moreover, this research (which has the advantage of being prospective rather than retrospective) establishes that “developmental stress activates genetic propensities, and not that genetic propensities cause individuals to seek out stressful life situations, or otherwise ‘come to harm'”.
There is research in humans which suggests that carriers of this “low-function” allele, when exposed to stresses during childhood and adolescence (like maltreatment and/or abuse) are more vulnerable to suffer from depression, be more impulsive and be more disinhibited. Moreover, bulimic women with comorbid problems like anxiety and substance-abuse were also found to be more likely to have the “low-function” allele of the serotonin transporter gene.
Statistically, more likely strongly suggests that the “low-function” allele is strongly associated with an altered stress-response. BUT the fact that there are bulimicswithout comorbid anxiety and/or substance-abuse (and all the other aforementioned traits common in BN and AN-BP) illustrates that the “low-function” allele is not the whole story. It doesn’t “cause” these traits in the literal sense, but it may play a big role. In other words, it is part of the story.
Steiger et al. stress that “in the bulimic population, anomalies in [serotonin] activity are observed to predict severity of concurrent psychopathological trait manifestations far more consistently than they do for severity of bulimic symptoms… ”
So, what is the take-home message about the role of serotonin in bulimia nervosa and binge-purge type anorexia?
An implication is that [serotonin] alterations may not directly cause bulimic eating problems, but may rather indirectly influence susceptibility to bulimic syndromes, by heightening traits (such as affective instability or impulsivity) that play indirectly into risk. We also assume that abnormal [serotonin] status in bulimic individuals reveals an “end state” associated with diverse causal paths sometimes reflecting the cumulative effects of chronic dieting, sometimes a constitutional tendency based on heredity, sometimes the consequence of exposure to intense developmental or current stress, and sometimes a combination of all these things.
Of course, this has really important implications for treatment: individuals for whom abnormalities in the serotonin system are secondary (ie, consequences of dieting) might not require as extensive or prolonged treatment as those for whom serotonin dysregulation is more hereditary or for whom adverse events in childhood and adolescence might have activated the “low-function” serotonin transporter allele (or other genes in the pathway that may have the same end-result).
This is supported by a study (full text here) showing that traditional CBT seems to work well for bulimic patients with few psychiatric comorbidities but “enhanced” CBT is better suited for patients with a higher prevalence of psychiatric comorbidities.
In other words, the ultimate etiological model of the factors leading to disorders characterized by the presence of binge-eating and purging will come from “an understanding of the interplay among genetic factors coding for [serotonin] activity, environmental stresses that may amplify genetic susceptibilities, and environmental inducements toward dieting (which can be understood to indirectly reduce [serotonin] activity at a population level)” and this understanding will, hopefully, enhance the development and availability of more patient-specific treatment approaches.
References
Steiger, H.,, Bruce, K.R.,, & Groleau, P. (2010). Neural Circuits, Neurotransmitters, and Behaviour – serotonin and Temperament in Bulimic Syndromes Behavioural Neurobiology of Eating disorders , 125-138 DOI: 10.1007/7854_2010_88
A few things I am confused about. . . (Maybe I am just tired though!)
1. “In the well-established category is the role of serotonin in mediating harm assessment and harm avoidance. (In psychology, the term “harm avoidance” is much more complex than the literal definition of avoiding harm, it includes traits such as “excessive worrying; pessimism; shyness; and being fearful, doubtful, and easily fatigued”
I thought these traits were associated with high serotonin? (i.e. as in the Kaye at al. 2009 paper you cited in your AN summary?) — but then in the following paragraph you state that, “n the not very well-established category is the converse association of increased serotonin neurotransmission with behavioural inhibition, compulsiveness, inflexibility and enhanced vigilance”. Wouldn’t these traits be components of harm avoidance which is in the “well-established category and indicative if high serotonin?
2. “decrease tryptophan levels in the brain (and thus the synthesis of serotonin) increases bulimic urges (or depression) in bulimic and recovered bulimic individuals. (A similar study in anorexics have found that acute tryptophan depletion is anxiolytic – or anxiety reducing.” — this is REALLY interesting. Especially because tryptophan depletion ALSO causes occurrence of depressive symptoms in remitted depressed patients but NO mood change in healthy controls. These three different responses (increase in bulimic, anxiolytic or depressive states) to a single treatment in vulnerable individuals suggest these disorders are physiologically distinct but all act on the sertonergic system (or have some serotonergic influence). . .
3. You state, “research on nonhuman primates has shown that a particular version of the serotonin transporter gene (the one that gets serotonin back into the releasing (or presynaptic) cell), , termed the “low-function” allele, alters stress-response (and serotonin metabolism).”, but then “developmental stress activates genetic propensities, and not that genetic propensities cause individuals to seek out stressful life situations, or otherwise ‘come to harm’”.
Aren’t these converse statements? Either genetic propensities –> enhanced stress response or stress –> genetic propensities, or is this a cyclic relationship?
4. Ultimately, the entire post is VERY interesting — the correlation of BN to the low function allele would mean that there would be more serotonin in the extracellular space, available to interact with receptors. However, those with bulimia tend to display a mix of traits correlated with high serotonergic activity (i.e. compulsiveness, excessive worrying, rigidity) and low serotonergic activity (i.e. impulsiveness). I think you are right in that a “level” of serotonin or levels of a single protein (i.e. the serotonin transporter) cannot explain such a complex disorder — there are 15 subtypes of serotonin receptors and the interactions of serotonin with various receptors, distribution of receptors in brain regions, REGIONAL variation in serotonin concentration, upstream/downstream effects, make this system extremely complex. In addition, as you pointed out there is also huge heterogenity in builimic individuals.
5. “Statistically more likely strongly suggests that the ”low-function” allele is strongly associated with an altered stress-response. BUT the fact that there are bulimics with comorbid anxiety and/or substance-abuse (and all the other aforementioned traits common in BN and AN-BP) illustrates that the “low-function” allele is not the whole story.” — did you mean WITHOUT here?
This is a fantastic post (serotonin is my thing as you know! 😛 )
A:)
Hey A:), thanks for your thoughtful comment!
I’ll tackle your points in order.
1. Right, I should remove the word “conversely” there, it is confusing and not what I meant. It seems that it is well associated with harm avoidance, but I’m not sure how much those other traits fall under “harm avoidance” (I simply don’t know – I’m going based on the paper). I think it is less well-established that high serotonin is associated with those other traits I mention. That might be just due to the way these things are tested, the questionnaire’s used, etc.. I don’t know, it is something I need to look into more. I think the general gist is that high-serotonin = anxiety, worry, shyness, fear of uncertainty, and low serotonin = impulsiveness, thrill-seeking, extraversion?
What I meant to portray is the sentiments that Steiger et al has in that the association of high-serotonin with many of the aforementioned traits is sometimes an over-generalization, and gets stretched too far. I worded myself incorrectly. Thanks for pointing that out!
2. I read a few tryptophan depletion/alteration studies, but I need to read more. It is interesting, but the sample sizes are usually small, and I do recall coming across a few critical articles, mentioning some things that don’t seem to add up. Need to investigate more.
3. Okay, maybe I didn’t word myself well here either. I do mean it is a cyclical thing: an individual might have an altered response to stress – but, maybe at low levels of stress, it is not noticeable. Maybe it is not “activated” enough? Add to that basal altered stress response, you add stress during development, for example, and the system snowballs. That’s just one possible explanation. I think there are many more.
4. Exactly, and what about binge-purge type anorexics? What about people such as myself who cycle through AN, AN-BP and BN? The huge problem here is the completely arbitrary DSM classifications. My responses to specific situations don’t change very much, and yet I seem to fluctuate in diagnoses a lot. But, I think the fluctuation is rather artificial, ie: AN without BP was early stages of the disorder, or, when I’m doing well (accidentally losing weight, not on purpose, not psychologically restricting) or in long-term low-level stress situations. Not eating enough just seems to happen by accident now-a-days, but leads to weight loss (much much faster than it used to before, so last time I lost weight, it was totally unintended), and bingeing-purging happens when I’m acutely stressed, or other triggering emotional states.
The difference, then, between AN-BP and BN is just weight. Too long in AN-BP, and it is bound to become BN because I gain weight as a result of bingeing and purging. So, then what? where do I fit on the spectrum? I have my ideas and theories, but it is worthwhile to ponder: are we studying the right things? Are we categorizing individuals with EDs in a way that makes sense to really understand these disorders? I have my doubts.
For me, with regard to harm avoidance, for example, I have a lot of anticipatory worry and don’t do well with uncertainty (career/school-wise, especially). Sometimes these thoughts are pervasive enough to lead me to symptoms. But, I’m not shy – at all. Not even remotely. And I don’t get fatigued easily either, I sleep 6 or so hours a day, and feel fine (I sleep way more when I become unhappy). So, what to make of this variability? Things are complicated! I’m just one person, of course, but it illustrates that things really are complicated.
5. Yes! Without! Thanks!
Can you proof-read my posts before I publish them from now on ;-)?
Tetyana
Thank you for your resonse. Anything I can do to help families not experience what we have. I miss her every second of every day she was my best friend. Help me keep the dialogue going. I also have wristbands if anyone wants one just send the address.
Very interesting article. My daughter battled the disease for 7 years and lost the fight Oct 28, 2011 by hanging herself in her bedroom. Shelby was prescribed zoloft for years but wouldn’t take it because it didn’t have a nutrition label. After reading this article I am better able to grasp her last day. She was in a manic state but for 1 long year she only ate raw carrots and frozen peas. Towards the end the disease took her to a place of weirdness (without any other word to describe it) she wrapped her bag of frozen peas in 3 towels before putting them in the microwave. She would only use plastic spoons and would never use plates or bowls. The obsessions were scary to watch take over. I knew the end was near when her stomach was so swollen and her skin was orange. Her kidneys and liver were failing again, she knew it didn’t want to go back in the hospital so she left us. All of the doctors she has seen didn’t know what to do, the hospitals would release her because she was stable, residential facilities couldn’t keep her any longer because of money….now look where we are. I feel that I could school all of the doctors in this disease. The progression is different when you are living with it day after day. Preparing youself for your child to die year after year, doesn’t help because once it happens there is no preparing for living without your child or without the disease. Caring for both of them gave me purpose. I miss Shelby terribly but I also miss everything else too even the disease. Thank you for readng my thoughts. Please go to Kill Anorexia with Kindness Shelby Wright Memorial.
Roxanne, I’m terribly sorry for your loss 🙁 I don’t really know what to say – this disorder is awful, the effects it has on the sufferer and the sufferer’s family and caregivers is just as awful – it is terrifying, really. I’m really sorry that you’ve had to endure it, and watch your daughter suffer through it. It is terrible 🙁
Thank you for taking the time to comment, it is really important and I really appreciate it.
I fixed the URL link so that it links to the Facebook page (it was broken).
oh, god, Roxanne. I am so sorry for your loss. I just went to your memorial because my heart caught in my throat at her name…I was at center for discovery with your daughter years ago. I am so, so very sorry to hear this.
Wait you bought that book? It’s so expensive…
It is free (online PDFs, not the print copy) if you have institutional access, which I do through the University of Toronto.
Jelly!
That *always* makes me laugh! I can forward it to you if you want.
I would be very grateful if you did (and just the resources you use generally)!
how do i access just your dropbox/not a specific file? thank you!!
This was not a topic I was very familiar with but found it interesting. After reading combined with what I already know about serotonin it only makes since that an imbalance could cause such a serious condition. Given the fact that this would cause depression and then effecting a persons self image.
I appreciate this and all the comments, I suffered from bulimia for 6 years. I finally recovered with the help of someone who reacted the opposite way of the way I thought everyone would respond if I had told them about my illness. He presented me with kindness and persistence. He had accepted he did not understand, but this drove in him a greater urge to read and inform himself about what I was going through and learn all the ways he could help. Most others did not understand. They believed it was merely a product of self-consciousness and insecurity and that if I realized I was “not fat” I would be able to recover. This couldn’t be more far from the truth, and shedding light on that myth with this post makes me extremely happy. I have now been 10 months recovered, my recovery has been possible I believe with the help of the anti-depressant Wellbutrin (and a new found interest in lifting). Since I started taking the drug, I seldom have any urges to binge and purge or to starve. I truly believe that if I had not had this wonderful man in my life for three years, continually helping me every single day, who had forced me to seek professional help multiple times and finally get me on anti-depressants, I would have been dead from the product of this disorder, or have succeeded in one of the attempts of taking my own life. I am sad to say that he is no longer in my life, for we are no longer together and I wish every day he could see what his hard work hard work has done–given me life again.
Excuse me if this is a silly question, but is it likely that the supplementation of l-tryptophan or 5-htp would be helpful for bulimic patients?