This is part III of my series on the role of dopamine in anorexia nervosa. In my first post I did a little introduction on dopamine and dopaminergic signalling. In the second post I talked about preclinical studies that used animal models of anorexia nervosa. In this post I’ll briefly go over some of the research that has used patients with anorexia nervosa to understand the role of dopamine in this disorder.
I’ve got to be honest here: I wish things were simpler. I wish the research wasn’t so contradictory–but it often is. When you first start to explore a topic, and you are not even sure you are asking exactly the right question, things often look messy. I find this is true for my own research as well, and as a graduate student, it is hard to accept contradictory results. Yet, it is also hard as a science blogger to write about contradictory findings because it can be confusing, and messy.
But, stay with me. I’ll try to make it as simple as possible.
In the last post I concluded by saying that despite some contradictory findings, the majority of the studies seemed to point to the conclusion that in animal models of anorexia nervosa there was increased dopaminergic activity. What about human studies?
One way to study dopamine activity in anorexia nervosa is to study its role indirectly: by looking at the levels and activity of hormones regulated by dopamine. For example, dopamine inhibits the release of prolactin, a protein that’s involved in lactation (among other things),
Similarly, should anorexia be associated with increased dopaminergic activity, prolactin levels would be decreased, postsynaptic dopaminergic receptors should be downregulated, and the prolactin response following the administration of D2 receptor [blocker] should be decreased.
One study found this to be the case: the prolactin response following administration of a D2 receptor blocker was blunted. But another study found that this decreased response depend on weight–which means that maybe this doesn’t have much to do with causing anorexia nervosa, but it is a by-product of the low weight.
In reviewing similar studies, the authors of this paper concluded that,
… the findings in AN involving the secretion of growth hormone and prolactin could be concordant with the hypothesis of an increased central dopaminergic neurotransmission… However, there is no convincing evidence that increased dopamine underlies the entire endocrine dysfunction of the disorder.
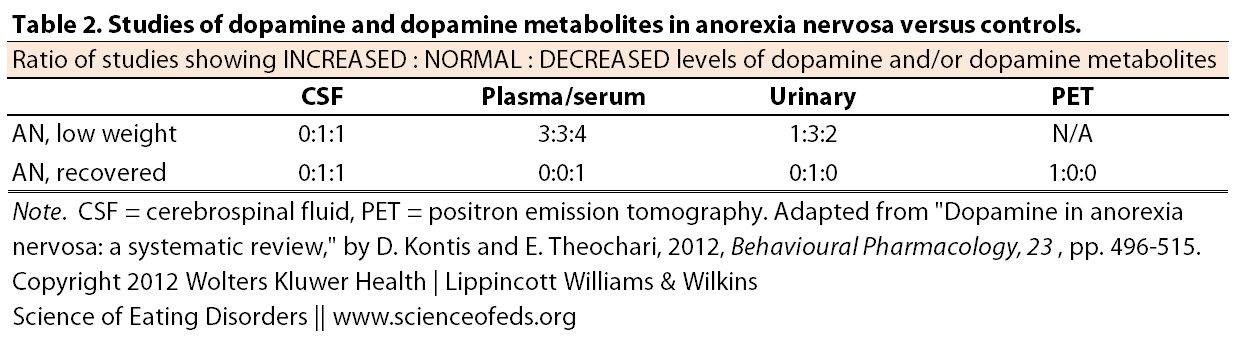
Besides looking at hormones regulated by dopamine, scientists can also look at dopamine itself or dopamine metabolites (by-products of dopamine metabolism) in the cerebrospinal fluid (CSF), plasma or urine. As you can see, the findings from studies doing just that are contradictory. In the table below I highlighted the ratio of studies showing increased to normal to decreased levels of dopamine in AN patients and recovered AN patients.
For example, in low-weight (as opposed to recovered) anorexia nervosa patients, summarizing the studies looking at dopamine/dopamine metabolites in plasma/serum reveals that there’s a fairly equal number of studies that show an increase, decrease, or normal levels, compared to healthy controls.
The authors of this review suggest that one of the reasons for these discrepancies might be because of the all the different ways and conditions under which the dopamine and/or dopamine metabolites were measured.
One neuroimaging study by Frank et al (2005) found evidence that suggests there might be decreased dopamine at the synapse, and thus increased dopamine receptor density (or affinity). In this case, the receptors in question are the D2/D3 receptors. So maybe this is the study that started the odd myth that increased dopamine receptors CAUSE anorexia nervosa.
But keep in mind: Frank and colleagues looked at 10 women who had recovered from anorexia nervosa and compared them to 12 healthy controls. It is just one study, and it is also not a prospective study. To determine whether this difference caused anorexia nervosa, we’d have to rule out a lot of other possibilities and show that this increase coincided with, or pre-dated the onset of anorexia nervosa. This study simply looked at women who had recovered from anorexia nervosa (however that was defined).
In the conclusion part of the abstract, the authors do not mention cause:
These data lend support for the possibility that decreased intrasynaptic [between synapses] [dopamine] concentration or increased D2/D3 receptor density or affinity is associated with AN and might contribute to the characteristic harm avoidance or increased physical activity found in AN. Most intriguing is the possibility that individuals with AN might have a [dopamine] related disturbance of reward mechanisms contributing to altered hedonics of feeding behavior and their ascetic, anhedonic temperament.
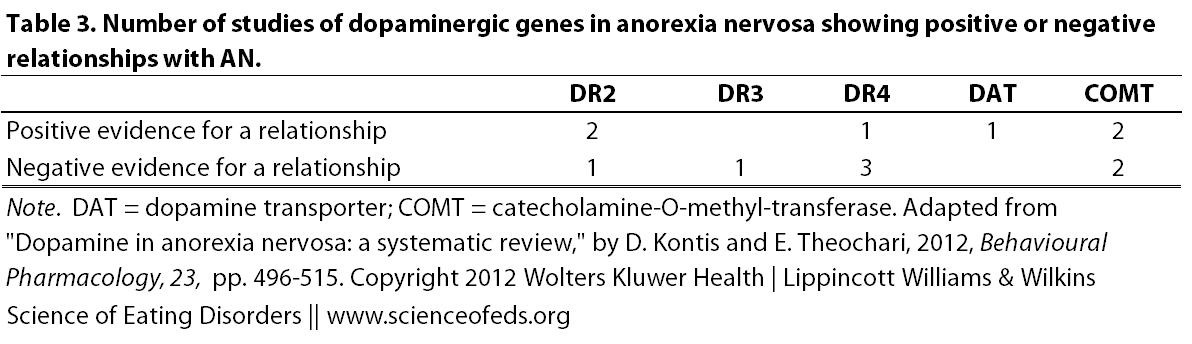
The other thing that scientists can do is see if the dopamine receptor genes (or genes involved in dopamine transport or metabolism) are somehow different between patients with anorexia nervosa and healthy controls. The data here are again mixed (DR = dopamine receptor).
DR2, DR3, DR4, DAT, and COMT are different genes that researchers have analysed to see if there are any differences between the versions of the gene (called “alleles“) that patients with anorexia nervosa have compared to the normal population. As you can see, some studies found a positive relationship between a specific version of a gene and anorexia nervosa, but others failed to find any differences between anorexia nervosa patients and control groups.
Science is messy.
Interestingly, there was a study in 2010 by Frieling and colleagues suggesting that epigenetics might play a role in altering dopaminergic genes and dopamine signalling in patients with anorexia nervosa. So, it might be that patients with anorexia nervosa have the same gene “versions” as those without anorexia nervosa, but the way they are regulated (ie “turned on” and “turned off”) might be different. Maybe we’ve been asking the wrong questions?
Kontis & Theocari conclude this section of their review by suggesting that it seems there’s good support for the role of the D2 receptor gene and the dopamine transporter (DAT) in anorexia nervosa, but the role of D3 receptor, D4 receptor, and COMT genes needs to be evaluated further. (Personally, I think they all need to be evaluated further.)
READ PART IV (TREATMENT with ANTIPSYCHOTICS) HERE.
References
Kontis, D., & Theochari, E. (2012). Dopamine in anorexia nervosa Behavioural Pharmacology, 23 (5 and 6), 496-515 DOI: 10.1097/FBP.0b013e328357e115
I find your research very interesting, as I have dealt with an eating disorder for almost 11 years. I have always believed that there is more of a biological cause to my behaviors rather than a psychological. My father is an anesthesiologist and has always a believes the same. Throughout the years, we have had tests done and about 3 years ago, my dopamine levels were through the roof. At the time, I was actively in my eating disorder and underweight. However, I actually came across this article because I was researching relations to HIGH prolactin levels and eating disorders. It appears that I not only have idiopathic hyperprolactinemia, but I also have high testosterone. I’m not sure if either of these have anything to do with my eating disorder and that is why I thought I would comment. Maybe you have come across something in your research that suggests such a thing?