Anxiety disorders (ADs) are common among patients with eating disorders. In one study of female inpatients, around 50-65% had a comorbid anxiety disorder (see my post here). Anxiety disorders in patients with anorexia nervosa (AN) typically begin before the eating disorder and often persist after weight restoration and recovery (Bulik et al., 1997; Casper, 1990). Moreover, previous twin studies have suggested that there’s a “correlation between eating disorders and certain anxiety and depressive disorders, suggesting they comprise a spectrum of inherited phenotypes” (Hudson et al., 2003; Mangweth et al., 2003).
In this paper, Michael Strober and colleagues hypothesized that anxiety disorders and anorexia nervosa share common genetic, neural, and/or behavioural mechanisms. As such, they sought to investigate the association of AN with ADs by studying the prevalence of ADs in first-degree relatives of AN patients and comparing it to the prevalence of ADs in first-degree relatives of healthy controls.
Their rationale was that,
If transmission of anxiety proneness plays a role in vulnerability to AN, it can be expected that anxiety disorders would aggregate significantly in family members of probands with this illness.
Just to note, this study only investigated the relatives of restrictive-type AN patients, and in addition to ADs, they included obsessive compulsive personality disorder (OCPD) (not to be confused with obsessive compulsive disorder (OCD)).
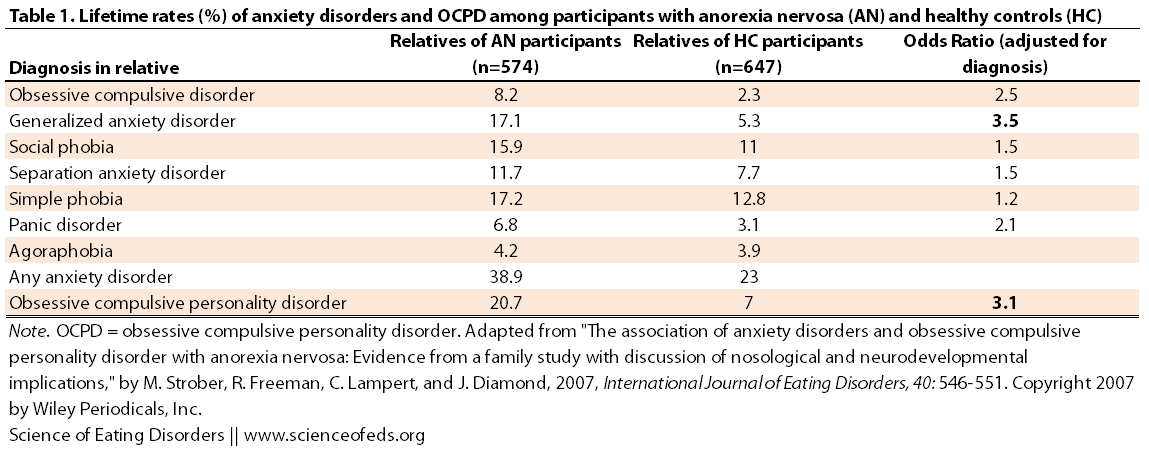
Here’s a table summarizing the prevalence of ADs and OCPD among relatives of AN participants and healthy controls, as well as the adjusted odds ratio.
The prevalence of OCD, generalized anxiety disorder (GAD), any anxiety disorder, and OCP was significantly higher among first-degree relatives of AN patients than healthy controls. Indeed, first-degree relatives of AN patients had a 3 times greater risk of having OCD, GAD, and OCPD, and a moderately elevated risk of panic disorder, social phobia, separation anxiety and simple phobia.
When the authors controlled for the fact that relatives of AN patients have a higher risk of full or partial EDs, they still found that GAD and OCPD were much more prevalent among relatives of AN patients than controls (p<0.001 for the nerds).
There are several limitations to this study, but the main one, I think, is that the authors screened for psychiatric illnesses in the healthy control participants, and in doing so, they might have increased the apparent association between ADs and AN.
The authors went on to speculate about what these findings might mean for the pathophysiology of AN and the implications for nosology (classification) of AN.
Specifically, the authors hint at the idea of potentially classifying AN under ADs. (“The findings also invite speculation on a possible nosological relationship of AN to anxiety states.”) I am not sure how I feel about that, although I do think there are a lot of similarities. Mainly, though, I need to read more about this topic to formulate an educated opinion. (And there are lots of papers, here’s a relatively recent one, for example, which is freely available to the public.)
On how anxiety disorders and anorexia nervosa might be linked on a genetic and neurobiological level, Strober et al. wrote:
Given that persons with behavioral inhibition, aversion to novelty, and neuroticism (traits which, as noted earlier, occur premorbidly in AN) are prone to low self-regard and thus experience higher than normal levels of perceived stress, these findings collectively support the intriguing possibility that vulnerability to AN is expressed neurodevelopmentally; specifically, that risk unfolds in a manner that is dynamic and progressive, involving a heritable inclination to extreme anxiety and fear, and then compromise of emerging cognitive and affective processes by corticolimbic circuitry that is, in effect, ‘‘locked’’ in a state of chronic activation by life events that are perceived and experienced by these temperamentally ‘‘at risk’’ children as uncomfortably novel and anxiogenic.
The authors concluded with a question, “Importantly, what factors contribute uniquely, or selectively, to weight and shape concerns among those who are anxiety prone?”
Readers, what are your thoughts on this?
By the way, ELT makes her case for anorexia being an anxiety disorder “with a specific set of rules” in her guest post on Charlotte’s blog (Anorexia Nervosa: An Anxiety Disorder with a Specific Set of Rules?). I urge readers to check it out, ELT’s experiences are–while not unique–under-represented when we talk about eating disorders and eating disorder causes (particularly in the mainstream media).
References
Strober, M., Freeman, R., Lampert, C., & Diamond, J. (2007). The association of anxiety disorders and obsessive compulsive personality disorder with anorexia nervosa: Evidence from a family study with discussion of nosological and neurodevelopmental implications International Journal of Eating Disorders, 40 (S3) DOI: 10.1002/eat.20429
Synaptic plasticity alters when cyto-skelteton remodels in dendrite spines. Anxiety is tied to plasticity.
Cofilin 1 is the key morphological gene of dendrite spines. A cofilin variant may be how AN anxiety takes time to show up.
The early developmental stages of the brain mask pending dendrite morphology. Which means, unlike the amygdala, it is the ventral hippocampus which comes on to play a controlling role regarding one’s level of anxiety. See 2010 “Hippocampal NMDA receptors and anxiety….” (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824088/) …”Regressive neuronal changes occur in humans who experience greater psychological distress.
Quoting 2010 “Association of Anxiety and Depression With Microtubule….”(“http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2926797/)
Synaptic plasticity
As someone who works with a protein (a highly conserved serine/threonine kinase) that regulates neuronal polarity and synapse morphology, most likely via cytoskeletal regulation, I fail to see how this is relevant to the discussion. Cofilin is one of many, many, cytoskeletal regulators and I’m not sure I see the link here to the systems level phenotypes, given that there’s so much redundancy in cellular pathways. Anxiety doesn’t depend on cofilin more than anything else depends on proper neuronal morphology and activity.
(Just to add, 1/3 of my thesis is spent talking about how the cytoskeleton regulates neuronal polarity and synapse formation; and another huge chunk on how that regulation impacts behavioural phenotypes. My lab mostly studies regulators of neuronal development.)
“Cofilin 1 is the key morphological gene of dendrite spines.”
This makes no sense. Cofilin is an actin-binding protein, and sure it might regulate dendritic spines, but in all honesty, what DOESN’T regulate dendritic spines? Everything that’s linked to actin and microtubule networks can potentially regulate dendritic spines, for one. Neuronal activity regulates dendritic spines. And by the way, there are a lot of actin-binding proteins: http://en.wikipedia.org/wiki/Actin-binding_protein
I don’t mean to be rude, I just feel like what you wrote is nonsensical, for the most part. And whatever is there that makes sense focuses too much on a very tiny component of the picture, ignoring the rest.
“… very tiny component of the picture….” Yes, there’s always more of the “rest”.
“Anxiety doesn’t depend on cofilin …” underplays the nano-biologically of involved cells.
Yes, there’s “many, many, cytoskeletal regulators” & my writing “key” merits editing.
Since AN doesn’t show up in infancy/early the “redundancy” of “neuronal development” implicates some time delayed program of processing anxiety level.
Cofilin 1, being an actin de-polymerizing factor shows up in mice (yes, humans are not mice) as a quantitative trait loci for level of anxiety suspect. See fall 2012 “Cofilin-1: A Modulator…
(“http://www.plosgenetics.org/article)/info%3Adoi%2F10.1371%2Fjournal.pgen.1002970)
Good post,as usual!
Thanks for quoting my blog post on Charlotte’s blog, Tetyana – and in particular, making a point that my experience, while not unique, is under-represented – especially in the media.
Cathy aka ELT.
As someone who suffered from an eating disorder in early teenage years, I have a lot to say about this blog post. I believe that Anorexia is not an Anxiety Disorder, however I do believe that they are directly related. When one has an eating disorder their anxiety increases when asked to do certain things, for example eating “fear foods” or retraining from Ed behaviors. Anxiety plays a big role in how one with an eating disorder thinks. If something they do gives them anxiety they are more likely not to do them.
In conclusion, I do believe that anxiety disorders and eating disorders play hand and hand, I do not go as far to say they are the same thing or a type of an anxiety disorder. Eating disorders in my opinion are in their own category in mental diseases and should stay that way.
Yeah, I do agree that they are not the same thing, but there’s more overlap than just food/weight-related anxiety during the acute phase of the eating disorders, as anxiety disorders often precede ED onset and continue after ED recovery.
I honestly haven’t thought of it this way before…is it possible to think of 2 “groups” of AN? The “anxious subtype AN” and “depressive subtype AN” so to speak…purely from observation (not research), I’ve seen lots of instances where AN seems almost a symptom of depression or a symptom of anxiety, and behaviors seem different based on the type. E.g., anxious AN patient obsessively calorie counts/hides food/secretly exercise vs depressive AN patient isolates/sits through silent meals/refuses eating. Sorry – this thought literally just popped into my head so it could be invalid.
Well, you can subtype individuals with EDs on all sorts of ways, really. Although I’m not sure to what extent you can group them into anxious subtype and depressive subtype, given how frequently they co-occur.
The examples you brought up (re: anxious AN patient obsessively calorie counts/hides food/secretly exercise vs depressive AN patient isolates/sits through silent meals/refuses eating) are all food-specific, whereas anxiety and depression, if they are comorbid in AN, would have to be non-food/ED specific, otherwise it is just not clear whether it is not actually depression per se, but AN (or starvation)-induced low mood.
If AN was a symptom of depression, I wouldn’t call it AN, I’d just call it depression-induced lack of appetite, and same with anxiety.
Moreover, the examples you bring up, like refusing eating, or being silent, aren’t really markers of depression, and I don’t think hiding food or calorie counting aren’t markers of anxiety either, and certainly they co-occur (counting calories and, say, isolating).
True – I didn’t really think it through. Thanks for clarifying!
🙂
Looking forward to your posts!
Have often thought myself it would be useful to subtype via aetiology rather than overt symptoms, as this could help in treatment, but then asking an anorexic why they’re doing what they’re doing will be fruitless (if my younger self is anything to go by – I assumed I had a brain disease because I had no concept that emotions were involved and was not aware at that age that psychological problems meant emotional problems, it would not have occurred to me). But some keen assessment of ‘why’ – perhaps on a social level – could help with treatment plans. You examples of the secretive hiding (not wanting people to know you are ill out of fear of intrusive care seeking) and the sullen sitting through meals (coercively making a bit shout about the fact you are ill, inviting conflict…) could be interesting in a different sense…