Eating disorders are mental disorders with physical complications. Sometimes lots of them. I’ve blogged before about medical complications that are likely to come up in an emergency room setting, but that was a while ago. So I thought today I’d focus specifically on medical complications that occur in bulimia nervosa (BN) as a result of purging (self-induced vomiting, laxative abuse, and diuretic abuse).
These complications are particularly important because patients with BN often appear healthy and can thus more easily hide their disorder, meaning that treatment is often initiated many years after disorder onset, and the duration of BN is often long, with recovery rates far lower than they should be (in one study, the 5-year recovery rate was a little more than 50%), which means that these complications can persist for many years.
I’ll go through some of the complications of self-induced vomiting, laxative abuse, diuretic abuse, and briefly mention some complications in patients with type 1 diabetes.
I. COMPLICATIONS OF SELF-INDUCED VOMITING
Oral complications of self-induced vomiting:
- cheilosis (painful lesions at the corner of the mouth)
- pharyngeal soreness (soreness at the back of the throat from the acidic stomach contents)
- dental erosions, dental cavities, and periodontal disease (“inflammation and infection that destroys the tissues that support the teeth, including the gums, the periodontal ligaments, and the tooth sockets”)
- enamel destruction/erosion, often resulting in thermal tooth sensitivity
- gingivitis (gum disease, a form of periodontal disease)
- sialadenosis (enlargement of the salivary glands (parotid swelling)
These can occur as early as 6 months following the onset of bingeing/purging. It is hard to predict the degree of the damage any individual patient with experience because it depends on the duration of the disorder, frequency of purging, types of foods consumed, and for the tooth related ones: quality of tooth structure (genetics is at play here) and oral hygiene.
Interestingly, the causes of parotid swelling (sialadenosis), which is rather common, are not well understood:
Some investigators think that the swelling is a direct result of binge eating, which often involves highly caloric foods consumed in very large quantities over short periods. Others postulate that chronic regurgitation of acidic gastric contents is responsible. Still others believe that pancreatic proteolytic enzymes brought into the mouth during vomiting stimulate lingual taste receptors; increased autonomic stimulation would thus cause the salivary glands to swell.
Esophageal and GI complications of self-induced vomiting:
- Esophagitis, esophageal erosis, ulcers, and bleeding (thought to result from the contact between acidic contents of the vomit with the esophageal mucosa)
- Heartburn and acid-reflux symptoms (often a sign of the above)
- Mallory-Weiss tears (minor self-limited bleeding, goes away on it is own if you abstain from bingeing/purging)
- Spontaneous reflux of acidic contents into the lower esophagus can also occur (because the lower esophageal sphincter gets lax)
- Esophageal strictures (narrowing or tightening of the esophagus)
- Esophageal rupture (though rare, it is fatal in approximately 20%; classic symptoms include: severe chest pain, painful swallowing, rapid breathing, rapid heart beat)
Interestingly, esophageal motility and gastric emptying seem to be pretty normal in BN patients (whereas gastric emptying is often delayed in AN patients).
Other complications:
- Not really a complication, but Russell’s sign and other abrasions/calluses are common dermatologic signs of purging
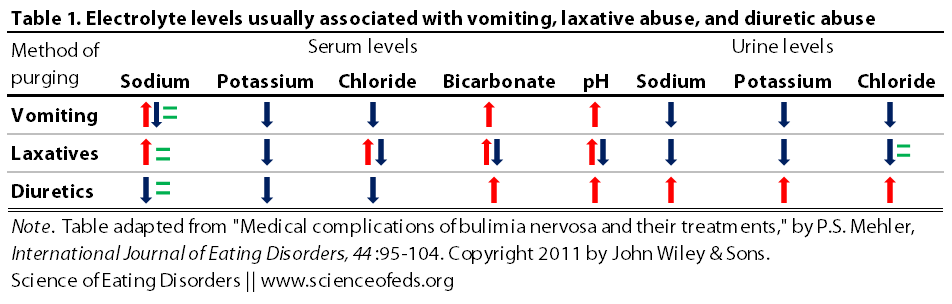
- Electrolyte abnormalities (see graphic below)
- Using ipecac syrup to induce vomiting can be toxic and fatal:
Ipecac has five alkaloid constituents (the major ones are emetine and cephaeline), all of which are toxic to cardiac and skeletal muscle. A 30-mL bottle of ipecac contains 21 mg of emetine. Because of ipecac’s long half-life (56 h), repeated ingestions can result in potentially fatal cumulative dose of emetine, variously reported to be between 500 and 1,200 mg. An irreversible cardiomyopathy with resultant symptoms of congestive heart failure, ventricular arrhythmias, and sudden death may follow.
II. COMPLICATIONS OF LAXATIVE ABUSE
There are five major classes of laxatives, and unfortunately, the ones that are most abused by BN patients (stimulant laxatives) are also the ones that come with the most medical complications.
GI complications of laxative abuse:
- melanosis coli (disorder of the pigmentation of the walls of the colon, generally benign)
- cathartic colon (result of habitual long-term stimulant laxative use, leads to dilated, atonic (without tone) colon; the colon can become “relegated to an inert tube, incapable of propagating fecal matter”
- functional impairment (where the loss of normal colon function is so severe that it requires surgery and an ostomy bag to treat the condition)
As with the other complications, there is a lot of variation between individual susceptibility to the effects of laxative abuse. It is not possible, yet, to predict which patients will experience what effects, and when.
Moreover, laxatives are generally ineffective (but clearly very damaging) method of purging. Only about 10-12% of ingested calories are lost. This is because laxatives have little effect on the small intestines where most of the calorie absorption occurs.
Systemic complications of laxative abuse:
- hypovolemia
- electrolyte disturbances (see graphic below)
III. COMPLICATIONS OF DIURETIC ABUSE
Diuretic abuse is less frequent than laxative use among BN patients, and like laxative abuse, it is also largely an ineffective method of purging. Most of the weight loss that results from diuretic use is water loss which can lead to dehydration and electrolyte disturbance.
The main problem with diuretic use is the cycle that one gets into:
The temporary loss of 2–4 pounds with consequent dehydration from the diuresis is followed by reflex fluid retention, weight gain, and the impulse to continue diuretics. Often, the initial stimulus to take diuretics is the normal fluctuation of weight from the fluid retention many women experience as part of the premenstrual syndrome.
Fluid and electrolyte abnormalities resulting from diuretic abuse:
- low potassium levels, low chloride ion levels and high blood pH (metabolic alkalosis)
- edema
- electrolyte disturbances:
The particular effects of diuretics depend on the class of diuretics used. For example, thiazide can lead to hypokalemia, metabolic alkalosis, hyperglycemia, hyperuricemia, hyperlipidemia, hyponatremia, and hypercalcemia. Whereas potassium-sparing diuretics can lead to hyperkalemia and metabolic acidosis.
In one study of ~950 individuals with eating disorders, 4.6% were found to have hypokalemia (low potassium). Hypokalemia was more prevalent among those with low mean body weight and low BMI, and who engaged in self-induced vomiting or diuretic abuse. Hypokalemia is particularly dangerous because it predisposes patients to cardiac arrhythmias.
The other common complication is pseudo-Bartter syndrome. It is characterized by hypokalemia, metabolic alkalosis, hypocholoremia, and hyper aldosteronism. This syndrome is seen in patients who self-induce vomiting, abuse laxatives and/or diuretics.
Unlike AN patients, patients with BN do not have problems with bone health unless there is a history of AN. They also have normal complete blood counts. Moreover, although irregular menses can occur during episodes of bulimia, future ability to conceive does not appear to be impaired.
IV. TYPE 1 DIABETES and EATING DISORDERS
I have blogged about this topic before (here), but it is well worth mentioning again. Disordered eating is unfortunately rather common among individuals with type 1 diabetes. Binge eating and insulin omission (insulin purging) occur in 30-50% and 30-40% of women, respectively. Naturally, these behaviours result in poor metabolic control.
Diabetic women who engage in these behaviors have been shown to have higher glycosylated hemoglobin levels, increased episodes of hypoglycemia and resulting hospitalizations for diabetic ketoacidosis (DKA), growth retardation and pubertal delay in adolescence, and increased microvascular complications, particularly retinopathy.
V.TREATMENT
I was going to do a little section about treatment but the treatment aspect of this paper is really geared toward clinicians, so I’ll just briefly mention a few suggestions that individuals can do themselves (those that do not involve medications).
For oral complications resulting from self-induced vomiting, Mehler suggests gentle brushing and use of fluoride mouth rinse immediately after vomiting to prevent cavities.
Laxative dependence is hard to treat, but the key is ample dehydration, high-fiber diet, and moderate amounts of exercise (provided there is no history of over-exercise). Be patient and be prepared for discomfort. Do remember that normal bowel function is defined as anything more than two bowel movements per week.
Potassium supplements and rehydration are important to correct hypokalemia. Mehler does warn that intravenous saline (to rehydrate the patient) be given at a slower rate than normal for bulimia nervosa patients because of the “risk for massive edema formation… due to their salt-avid state from the pseudo-Barteer syndrome.” So, if you or someone you know are in the emergency department for dehydration and/or hypokalemia, make sure that you (or they) are being administered saline at a lower rate to prevent severe edema.
Mehler concludes,
In summary, because the patient with bulimia nervosa may go unrecognized in healthcare settings and because their symptoms are relatively longstanding, it is important to be vigilant about the detection of bulimia in young patients with the aforementioned medical complications. Most of the medical complications of bulimia nervosa are readily treatable, but do require familiarity with the therapeutic interventions, to maximize their efficacy and help facilitate recovery.
References
Mehler, P. (2010). Medical complications of bulimia nervosa and their treatments International Journal of Eating Disorders DOI: 10.1002/eat.20825
I think people with EDs often have the “it won’t happen to me” attitude as far as health issues go. At least I know I did. Like, I wasn’t particularly concerned when I was diagnosed with osteopenia, and then full-blown osteoporosis. At the latter time, I was 16, and the consequences in my older years just seemed unimaginable. Part of that was being unable to see outside of the ED, and part of that, I believe, was due to my age. And at that point, I didn’t have any other irreversible health problems from my ED, at least, not as far as I knew of.
The scary thing about purging (vomiting), is that you really do not know what the consequences of doing it “just a little” are. I’ve never been diagnosed with BN. I didn’t start vomiting until I was 18. Even then, it wasn’t regular, and I’ve purged on and off, mostly off, since then. I mostly haven’t bothered with the purging because, for me, I do not lose weight, and I don’t end up expelling most of my food. It is certainly not anything I thought I’d get health problems from!
Long story short: in my early/mid twenties, my dentist took one look in my mouth, and asked me if I purged. The enamel is totally gone from my teeth, and I’m either going to have to get a full set of dentures or get a crown on every single one of my teeth (can we say expensive?). The enamel is not something that can just grow back. And as my case shows, you never know how much purging will cause problems. I’ve heard of women who died after just a few months of bulimia. And I know others, who have had bulimia for many years, and (say) they’ve never experienced a health problem from it. I always thought I’d be in that latter group. I certainly didn’t think such a small amount of vomiting would cause the extensive problems I know have.
This warning will most likely go unheeded, but what else can I do but try? 🙁