Eating disorder patients commonly complain of gastrointestinal (GI) symptoms including bloating, abdominal pain, and constipation. This is, of course, not surprising. After all, disordered eating behaviours such as self-induced vomiting, laxative abuse, and restriction are bound to have negative effects on the digestive system.
But just how common are GI complaints and functional gastrointestinal disorders (FGIDs) like irritable bowel syndrome among ED patients? And is there more to the relationship than simply ED behaviours causing GI disturbances? Luckily, a growing number of research studies are beginning to shed some light on these questions.
In a study published in 2010, Catherine Boyd and colleagues examined the prevalence of FGIDs among ED patients admitted to a hospital Eating Disorders Unit. They found that out of the respondents (73 in total), 97% had at least one FGID (as evaluated using the Rome II questionnaire). More specifically, on admission, 73% of the participants had esophageal disorders, 32% gastroduodenal disorders, 81% had bowel disorders, and 33% experienced anorectal disorders. At 12-month follow-up, the numbers decreased to 34%, 18%, 66%, and 18%, respectively.
Overall, despite significant improvements in weight, psychopathology, and disordered eating behaviours, 77% of participants had FGIDs at follow-up:
Neither change in BMI nor change in ED behaviors (self-induced vomiting, laxative use, and objective binge eating), and psychological variables (anxiety, depression, and somatization) had a significant interaction with change in individual FGIDs or in FGID regional categories from admission to 12-month follow-up.
In 2011, Dejong et al. published a study investigating the prevalence of irritable bowel disease in outpatients with bulimia nervosa. Out of 64 participants, 44 (68.8%) had IBS. This is compared to around 10-15% in the general population (in the US) (Saito et al., 2002).
That same year, Abraham and Kellow (2011) published a study looking at how FGIDs affect the quality of life among eating disorder patients. The prevalence of FGIDs was 93% in their sample. Interestingly, they found that only IBS, but not other FGIDs, correlated strongly with quality of life scores.
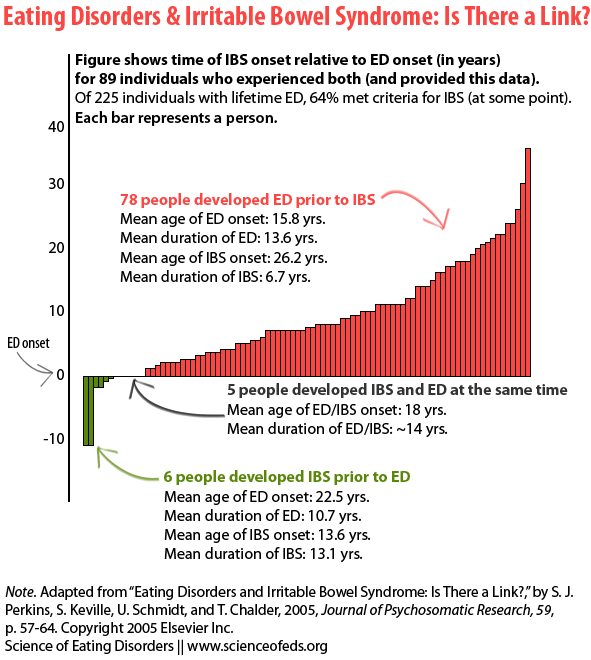
A couple of years prior to these studies, Perkins et al. (2005) examined the temporal relationship between one FGID in particular, IBS, and eating disorders. That is, in addition to determining the prevalence of IBS, they were interested in finding out what came first: the ED or the IBS. They were also interested in identifying any predictors of IBS symptoms among ED sufferers.
Perkins et al. hypothesized that the relationship between IBS and EDs might be more complex than meets the eye in part because
it is has been noticed that there are a number of shared demographic and clinical features between populations with EDs and IBS. Women are overly represented in IBS [8] and ED populations [15]. In addition, these two conditions have a high prevalence of physical and sexual abuse [12]. Finally, the individuals with these conditions tend to have personality characteristics of perfectionism, negative self evaluation, self-blame and feelings of ineffectiveness [16–20].
Out of 225 respondents, 64.4% had met the criteria for IBS (using the Manning criteria), although only 24.8% had been given a formal diagnosis of IBS. Out of the 89 participants who reported both the age of ED and IBS onset, 87.6% had an onset of their ED prior to IBS symptoms, 6.7% had onset of IBS prior to ED, and 5.6% had onset of EDs and IBS the same time (See figure below).
The bigger (longer?) the bar, the greater the difference (in years) between the onset of IBS and ED.
Note the difference in age of ED onset between those who developed IBS first and those who developed the ED first:
The group developing IBS after the onset of their ED had the typical teenage onset of their ED (mean age 15.8 years) and a lengthy time period between the onset of the ED and the IBS (mean 10.4 years). In contrast, the small group that developed IBS first had a late onset of the ED (mean 25.5 years).
Out of those reporting current IBS symptoms, 63% had a current ED.
What about predictors of IBS symptoms? Perkins et al. found that inappropriate laxative use was significantly correlated with severity of ED symptoms and the number of IBS symptoms. Neither ED duration nor lowest BMI predicted the number of IBS symptoms.
The high prevalence of IBS (and other FGIDs) among patients who have (at least to some extent) recovered from an eating disorder ED populations is interesting. Perkins et al. suggest that perhaps “hyper-vigilance to internal sensations” has a part to play in this.
Just as FGIDs are overrepresented in ED populations, EDs are overrepresented in FGID populations: In a study of 127 patients seeking treatment for an FGID, 15.7% were found to have a history of an ED (Porcelli et al., 1998).
Taken together . . . , our findings suggest that EDs may be predictive of the later development of IBS, irrespective of the persistence of the ED symptoms, but that where there are current EDs, the severity of these correlates with the number of IBS symptoms.
While disordered eating behaviours and other ED symptoms clearly play a role in GI disturbances, it is possible that other factors, such as chronic stress and personality traits, may play a role in causing and/or maintaining EDs and FGIDs:
There seems to be considerable overlap between the personality and early developmental factors cited as increasing the vulnerability to both types of disorders, such as anxious-avoidant personality type or childhood trauma [14,35]. Moreover, recent models of IBS [13] and of AN [36], which have tried to integrate findings from psychological and neurobiological research, have highlighted the pivotal role of chronic stress in the origins and maintenance of both disorders, with a combination of central and peripheral mechanisms working in tandem.
All of this is quite interesting and I look forward to future research exploring the relationship between GI symptoms and EDs. (Or perhaps it is already out there and I just haven’t looked hard enough? This is very possible.)
Importantly, a lot of these studies relied on self-reported questionnaires and potentially biased samples, so caution is warranted when interpreting these results (and extrapolating to other populations).
Finally, although it is a bit out-of-date now, Zipfel et al.’s 2006 review of gastrointestinal disturbances in eating disorders is quite good. I couldn’t find a pdf online, so drop me a line if you are interested.
References
Abraham, S., & Kellow, J. (2011). Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. Journal of Psychosomatic Research, 70 (4), 372-7 PMID: 21414458
Boyd, C., Abraham, S., & Kellow, J. (2010). Appearance and disappearance of functional gastrointestinal disorders in patients with eating disorders. Neurogastroenterology and Motility, 22 (12), 1279-83 PMID: 20718945
Dejong, H., Perkins, S., Grover, M., & Schmidt, U. (2011). The prevalence of irritable bowel syndrome in outpatients with bulimia nervosa. International Journal of Eating Disorders, 44 (7), 661-4 PMID: 21997430
Perkins, S.J., Keville, S., Schmidt, U., & Chalder, T. (2005). Eating disorders and irritable bowel syndrome: is there a link? Journal of Psychosomatic Research, 59, 57-64 DOI: 10.1016/j.jpsychores.2004.04.375
“Overall, despite significant improvements in weight, psychopathology, and disordered eating behaviours, 77% of participants had FGIDs at follow-up”
Oh God, I hate to be gross and TMI, but does this mean I’m likely never gonna be able to go to the bathroom like a normal human being again? I mean okay 77% =/= 100% but still, the other numbers and such are just…..uuugggh. And I never even touched stupid laxatives :/
As someone with a history of IBS (and coming from a long lineage of family members with IBS), symptoms CAN improve when you attain a healthy BMI and recover from nutrient deficiencies. I hope this isn’t TMI, but I had some REALLY embarrassing issues in the past (like having to go home to change) that have largely resolved. Do I still get “gassy” and is my stomach easily upset? Yes, but nothing out of the ordinary for my family. I don’t have to worry about not being near a bathroom on a hike anymore, and that works for me!
Thanks for this post! I remember being terrified that I had something seriously wrong with me in the past (like Chron’s or Celiac’s). I had no idea the (gross) side effects of having an ED were pretty typical until I agonized over it needlessly.
No, not “never.” First, this was just at 12 month follow-up, so a year after. Plus, FGIDs (as evaluated by the Rome II criteria, too) include a lot of different things, so, it is not like all 77% couldn’t go to the bathroom like a normal human being. PLUS, it is not like all the 77% were recovered. They were just followed-up 12 months after either admission to EDU or discharge (I don’t remember offhand).
Still, I wonder if these numbers are higher than they really are because (1) of the population they are studying (all people who were admitted to an EDU) and (2) perhaps people with EDs *are* more vigilant and/or hypersensitive to various internal processes (re: “hyper-vigilance to internal sensations”).
Plus, some part of that population would have FGIDs irrespective of the ED, since the prevalence of them is around 10-20% (depends who/where you ask). So keep that in mind, too.
I had my eating disorder for several years, beginning in 1989. In 2007 I developed a digestive condition (IBS?), which has only just gone away in the last few months (heaven!), so I suffered with that for six years. I always wondered whether the digestive condition was related to how much I abused my body all those years ago.
Hmm, interesting. So how long was the time difference between the end of the ED and the onset of IBS/IBS-like symptoms?
I was very surprised that in the study it seems like the average was around 10 years. Hard to know if they are related (especially in any single case).
Wow. … My bulimia burnt itself out around 1996 (I never had any recovery treatment). The digestive condition started at the beginning of November 2006. I remember I was sitting in a pizza restaurant in Scotland when the symptoms first hit me (so the digestive condition lasted seven years, in fact, not six).
Why on earth would it take TEN years for one’s body to rebel against ED behaviour in this way?
Well, it could be that they are not related at all. I mean is FGIDs occur in up to 20% of the population, it is reasonable to assume that some people with EDs will have FGIDs by chance (i.e., unrelated to the ED). It is impossible to say in any individual case, of course. I, too, am surprised by the results. But a big part of it could be due to the sample bias AND due to the retrospective self-reporting of the data. Self-reporting is :/ and retrospective is double :/
Ah, this is interesting. I started getting IBS-like symptoms after developing my ED, but it got really, really bad in 2007 (around the same time the ED also got really, really bad), and although I’ve been at a healthy weight since 2010, it’s still much worse than before I got very unwell. While I was recovering from the AN I hoped it was just a result of crappy (lol) muscle tone in my digestive system etc, but apparently not so much. It’s really interesting to know that this isn’t uncommon. I think I quite look forward to future research on the links between EDs and digestive issues as well!
This is very surprising to me! As someone diagnosed with IBD as a very young child (colic that wouldn’t go away), I expected to find a stronger correlation between early GI upset and EDs. I sussed out that I made the connection as a kid that when my stomach was very upset, just getting the sickness over with would make me feel better, which likely contributed to future restriction and purging as I unconsciously turned that into a metaphor.
I’m glad there’s some research being done into this avenue, though I do have concern that the results here may be waved around in treatment settings a la “you’re just oversensitive because you abused laxatives” and diminishing the still-evolving biological cause.
Over three years since choosing recovery and my digestive system still doesn’t work properly. I still get bloated and gassy more than most people would.
That sucks Sarah. Is it for sure related to the ED? Have you had it checked out?
My doctor said it is likely that I have IBS caused by my eating disorder, which I had for ten years, so I could see how that might mess things up.
Yeah. I’ve been so frustrated lately trying to find information on GI issues in individuals with EDs… there’s almost nothing. It is maddening.
It’s odd because it is a part of the body SO affected by the eating disorder.
Yeah. It is very frustrating because of the (potential) implications for recovery. Some of the things that are recommended for people do to test for food sensitivities or foods causing digestive problems–like limiting your diet and reintegrating foods to test for sensitivities–are so counter to what you should be doing in recovery. So, there’s a conflict there. I think it would be useful to have some longitudinal follow-up studies… but it is mostly case studies or very small sample size studies. Gah.
I’m also noticing that your comments keep going to spam and I have to fish them out manually. I have no idea why that’s the case. If you don’t see your comments appear, that could be the reason.
Yes, when I went to my doctor I was also advised to keep a food diary and/or cut out foods to try and see what was causing my gas, when really, it was just recovery symptoms!
It’s been about 3 years since I’ve recovered from anorexia, bulimia and long term laxative abuse, and my intestines are still constantly bloated, painful and I am always constipated with chronic acid reflux and heart burn and doctors can’t seem to figure out what’s wrong with me. I sometimes go through vomitting spells that mimick food poisoning, except for it’s more like the food in my stomach turns rotten and toxic inside of me until it forces me to expell it.
I can’t digest most carbs because there is something wrong with the part of my intestine that digests carbs, atleast that’s what they found from organ screening . The only foods I don’t have a problem digesting are all animal products. They keep trying to blame it on H pylori or yeast or IBS but I think it’s just that I damaged my insides, besides none of my symptoms match h pylori or ibs properly. IBS is basically the diagnosis they give you when they don’t know what it is. Despite knowing instinctually that the problem is not h pylori, i tried naturopathic treatments twice and could never finish because it caused me so much pain and made me very ill.
So anyway, I’m one of those people who have never found the light at the end of the tunnel. When I wasn’t eating I was never in this much pain, but I keep going and I tell myself this pain I feel now is the result of 13 years of eating disorder, that is the consequence, so there is no way I am going back to it.
At this point i don’t have much hope that it will ever get better. I’ve tried everything that is recommended for IBS and all sorts of things, I live an extremely healthy lifestyle and have even tried all sorts of “cancer” cures – nothing helps my digestive system.
After a long time of eating without any rules or restrictions I then started to feel safe enough to start adjusting my “meal plan” and one of the first things I did was cutting out foods temporarily to see if anything was causing me pain.
My digestive problems have never gotten better since, but they were a lot worse. I was having really aweful symptoms such as anal bleeding, and those problems are resolved when I don’t eat gluten or wheat.
I couldn’t digest milk after my eating disorder either, but after a year of being on probiotics I reintroduced it and have never had a problem with it since.
There are a lot of things I cannot eat, but that has not triggered my eating disorder, I still eat a lot of food and enjoy it. I can’t eat gluten, I can’t eat most carbs, I can’t eat beans, nuts, most strongly flavoured fruits and vegetables or else it makes my symptoms considerably worse and my symptoms are pretty bad without eating those things. I have to live only on bland things like meat, cheese, dairy, oatmeal, sweet potatoes, and minimal vegetables like tomatoes, mushrooms and a few greens, and on good days when my instestines don’t hurt as much, I add in new veggies. I can get away with eating gluten free pasta, or even the odd wheat hamburger once in awhile, other than that, gluten AND gluten free products, even rice, cause me a lot of pain.
Sabrina,
Even though my symptoms are not as debilitating your own, I have also had issues with bloating and acid reflux. I also have issues with gas and fragmented bowel movements, and sometimes really painful stomach aches. I have had blood tests which reveal nothing and have had it dismissed as damage from my eating disorder/IBS. I may go back to push my case for further tests soon as it is really uncomfortable.
Strangely enough I have found that on my days off work, my stomach is usually fine, and that it is when I am at work. So maybe even a little stress is causing it to get a lot worse; that and/or getting up at different times (I do shift work and on late shifts or days off I get up very late – like midday – and on early shifts I start work at 7.30am). I have found that waiting and eating breakfast later so it is more like my normal schedule improves it slightly, so I think that not having a regular schedule really throws my digestive system off, but it can be really bad and I feel unwell with it. It also can happen on late shifts too which is why I mentioned stress.
But I don’t know…I just want a definitive answer rather than just maybes.
My husband has just been diagnosed with IBS, son has active restricting ED and sons had terrible colic as babies. When I looked at the wikipedia entry for IBS I was astounded at the number of words that were familiar from my ED research. Depression and anxiety seem to be huge factors in both. Serotonin levels are abnormal and SSRI drugs can improve or exacerbate symptoms depending on the type. Atypical antipsychotics Clozapine and Olanzapine can be helpful. Of course, there are many serotonin receptors in the gut and this may be why. This is all without taking all the information from the article above. There seems to be too much overlap to be a coincidence. Similar genes, different expression? Fascinating at one level, bummer on the other that both my guys are suffering.